Table of Contents
Sjögren’s Syndrome: Symptoms, Causes & Effective Management
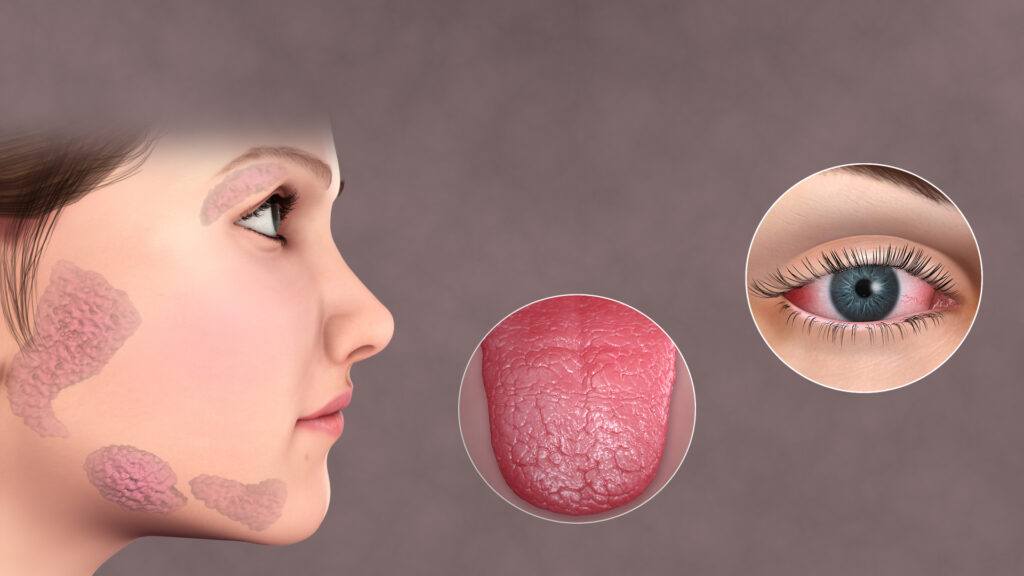
Sjögren’s syndrome is a chronic autoimmune disorder characterized primarily by dry eyes and dry mouth, caused by the immune system attacking moisture-producing glands. It can also affect other organs and significantly impact overall health and daily life. There are two types of Sjögren’s syndrome: primary, which occurs alone, and secondary, which occurs in conjunction with another autoimmune disease, such as rheumatoid arthritis or lupus.
Quick Facts
- Prevalence: Affects approximately 0.1-1% of the global population.
- Common Symptoms: Dry eyes, dry mouth, joint pain.
- Affected Population: Predominantly women over 40, though it can occur at any age.
Understanding Sjögren’s Syndrome
In Sjögren’s syndrome, the immune system mistakenly attacks the body’s tear and saliva glands, leading to reduced moisture production. The condition can exist independently (primary Sjögren’s) or alongside other autoimmune diseases (secondary Sjögren’s).
Common Symptoms
Recognizing early signs supports better symptom management:
- Persistent dry eyes, irritation, or gritty sensation
- Chronic dry mouth and difficulty swallowing
- Dental issues, including tooth decay and gum disease
- Joint pain, stiffness, and swelling
- Persistent fatigue
- Dry skin, nasal passages, and throat
- Enlargement of salivary glands
Causes and Risk Factors
The exact cause of Sjögren’s syndrome is unknown, but several factors contribute to its development:
- Genetic Factors: Increased risk if there’s a family history of Sjögren’s or other autoimmune conditions.
- Hormonal Influences: Higher incidence among women suggests hormonal factors.
- Environmental Triggers: Potential triggers include viral infections or prolonged stress.
Diagnosis
Diagnosing Sjögren’s syndrome typically involves:
- Medical History: Assessment of symptoms, family medical history, and presence of other autoimmune conditions.
- Physical Examination: Checking moisture-producing glands and joint inflammation.
- Blood Tests: Detecting specific antibodies (anti-SSA/Ro, anti-SSB/La), inflammatory markers.
- Eye Tests: Measuring tear production (Schirmer’s test).
- Salivary Gland Tests: Imaging studies or biopsies to confirm gland inflammation.
Effective Treatments and Management
Management focuses on symptom relief and preventing complications:
- Eye Care: Artificial tears, prescription eye drops, or punctal plugs to relieve dryness.
- Oral Care: Saliva substitutes, medications to stimulate saliva production, meticulous dental hygiene.
- Medications: NSAIDs for joint pain, corticosteroids, or immunosuppressants for severe cases.
- Lifestyle Adjustments: Increased hydration, humidifiers, regular dental visits, and balanced nutrition.
Potential Complications if Left Untreated
If untreated or inadequately managed, Sjögren’s syndrome can lead to serious health complications:
- Significant dental damage and tooth loss
- Eye complications, including corneal damage
- Increased risk of lymphoma
- Damage to organs such as lungs, kidneys, liver, and nerves
When to See a Doctor
Seek medical advice if experiencing persistent dry eyes, dry mouth, unexplained joint pain, or fatigue that interferes with daily activities. Early diagnosis and proactive management improve outcomes.
Practical Tips for Living with Sjögren’s Syndrome
Effective daily management includes:
- Regular use of moisturizing eye drops and oral hygiene products designed for dryness.
- Drinking adequate amounts of water to support overall hydration.
- Regular dental check-ups and consistent oral care routines.
- Using humidifiers at home or work to maintain comfortable humidity levels.
- Participating in gentle exercises and stress-reduction techniques such as yoga or meditation.
- Connecting with support groups for emotional encouragement and practical guidance.
Recent Research and Advances
Recent advancements in Sjögren’s research continue to improve treatment and understanding:
- Development of targeted biological therapies focusing on immune system modulation.
- Research on genetic and environmental interactions influencing disease progression.
- Improved diagnostic criteria and techniques facilitating earlier identification and treatment.
Frequently Asked Questions
Is Sjögren’s syndrome curable? Currently, there is no cure, but symptoms can be effectively managed to enhance comfort and quality of life.
Does Sjögren’s syndrome only affect the eyes and mouth? While dryness of eyes and mouth is common, Sjögren’s syndrome can also impact joints, skin, nerves, lungs, kidneys, and other organs.
Can diet influence Sjögren’s syndrome symptoms? A balanced diet rich in nutrients and hydration may support overall health, relieve symptoms, and minimize complications.
Additional Content
For comprehensive information on the various treatments you can explore our Autoimmune Disease Treatment page. If you are seeking expert medical advice, our Top Autoimmune Doctors section provides a list of highly recommended specialists. Additionally, for an overview of other autoimmune conditions, visit our Autoimmune Diseases page.