Table of Contents
Crohn’s Disease: Symptoms, Causes & Effective Management
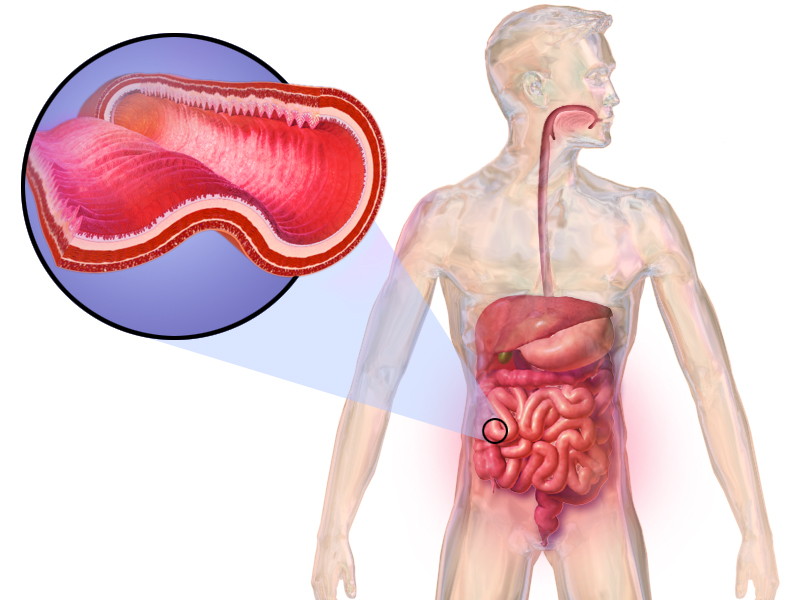
Crohn’s disease is a chronic inflammatory bowel disease (IBD) characterized by inflammation of the digestive tract, leading to abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition. It significantly impacts daily life, physical health, and emotional well-being, often requiring lifelong management and care.
Quick Facts
- Prevalence: Affects approximately 0.3% of the global population.
- Common Symptoms: Abdominal pain, diarrhea, weight loss.
- Affected Population: Can occur at any age but commonly develops between ages 15-35. Both men and women are equally affected.
Understanding Crohn’s Disease
Crohn’s disease causes inflammation of the digestive tract, potentially affecting any part from the mouth to the anus. The inflammation often spreads deep into affected tissues, causing severe discomfort, digestive issues, and potential complications such as intestinal narrowing and ulcerations. Unlike ulcerative colitis, which is limited to the colon, Crohn’s disease can occur in segments, interspersed with healthy tissue, resulting in a patchy pattern of inflammation.
Common Symptoms
Early identification of symptoms can greatly improve management outcomes and enhance quality of life. Common symptoms include:
- Persistent diarrhea, often severe
- Frequent abdominal pain and cramping
- Significant weight loss and reduced appetite
- Chronic fatigue and weakness
- Fever and general malaise
- Blood or mucus in stools
- Painful mouth sores
- Nutritional deficiencies due to malabsorption
Symptoms can fluctuate between periods of remission and flare-ups, affecting individuals differently.
Causes and Risk Factors
While the exact cause of Crohn’s disease remains unclear, researchers have identified multiple factors contributing to its development:
- Genetics: A family history of this disease or other autoimmune conditions significantly increases risk.
- Immune System: An abnormal immune response leads to chronic inflammation, causing the immune system to mistakenly attack the digestive tract.
- Environmental Factors: Diet, smoking, stress, certain medications, and exposure to infections or environmental toxins can trigger or exacerbate symptoms.
Diagnosis
Diagnosing Crohn’s disease typically involves several key steps:
- Medical History: A thorough evaluation of symptoms, their duration, family medical background, and dietary habits.
- Physical Examination: Checking for abdominal tenderness, bowel sounds, signs of nutritional deficiencies, and overall physical health.
- Laboratory Tests: Blood tests to detect inflammatory markers, anemia, nutritional deficiencies, and stool tests to rule out infections.
- Imaging Studies: Colonoscopy, endoscopy, capsule endoscopy, and imaging like CT scans or MRIs to visualize inflammation, ulcers, fistulas, or strictures.
Effective Treatments and Management
Effective management strategies focus on reducing inflammation, controlling symptoms, and preventing complications:
- Medication: Anti-inflammatory drugs (such as aminosalicylates), corticosteroids, immune system suppressors, antibiotics for infections, and biologic therapies targeting specific inflammation pathways.
- Dietary Adjustments: Customized nutritional plans, including potential dietary restrictions and supplementation, help manage symptoms and improve nutritional status.
- Lifestyle Changes: Stress reduction techniques, regular moderate exercise, maintaining proper hydration, and smoking cessation are crucial for symptom control.
- Surgical Intervention: Surgery may become necessary to address severe complications, including bowel obstruction, perforations, fistulas, or severe infections not responding to medication.
Potential Complications if Left Untreated
Without proper management, Crohn’s disease can lead to serious complications:
- Intestinal obstruction: Narrowing of the intestines causing blockage (strictures).
- Ulcers and fistulas: Formation of abnormal connections between organs or skin, causing severe infections.
- Malnutrition: Persistent inflammation impairs nutrient absorption.
- Colon cancer: Long-term inflammation significantly increases cancer risk.
- Severe infections: Resulting from compromised intestinal lining and immune function.
When to See a Doctor
It’s essential to seek medical attention if you experience persistent diarrhea, abdominal pain, unexplained weight loss, or rectal bleeding. Early diagnosis and treatment initiation greatly enhance symptom control, quality of life, and long-term health outcomes.
Practical Tips for Living with Crohn’s Disease
Effective daily management can significantly improve quality of life:
- Adhere strictly to medication schedules and attend regular medical appointments.
- Follow a personalized nutritional plan designed by healthcare providers or dietitians.
- Maintain good hydration, especially during flare-ups or episodes of diarrhea.
- Utilize stress management techniques, such as mindfulness, yoga, meditation, or cognitive behavioral therapy.
- Engage with support groups to gain emotional support, share experiences, and learn effective coping strategies.
Recent Research and Advances
Current research continues to improve understanding, diagnosis, and management:
- Advancements in targeted biologic therapies specifically designed to reduce inflammation.
- Ongoing studies exploring the role of the gut microbiome and probiotics.
- Innovations in minimally invasive surgical techniques, improving recovery times and outcomes.
- Research into genetic and environmental interactions contributing to Crohn’s disease.
Frequently Asked Questions
Is Crohn’s disease curable? Currently, there is no cure, but treatments effectively manage symptoms, reduce complications, and significantly improve quality of life.
Can diet alone manage Crohn’s disease? Diet plays a vital role in managing symptoms and supporting overall health; however, diet alone generally cannot completely control inflammation.
Is Crohn’s disease hereditary? Yes, genetics significantly influence risk, with family history markedly increasing the likelihood of developing Crohn’s disease.
Additional Content
For comprehensive information on the various treatments you can explore our Autoimmune Disease Treatment page. If you are seeking expert medical advice, our Top Autoimmune Doctors section provides a list of highly recommended specialists. Additionally, for an overview of other autoimmune conditions, visit our Autoimmune Diseases page.