Table of Contents
Understanding Autoimmune Vasculitis
Autoimmune vasculitis is a group of disorders characterized by inflammation of the blood vessels due to an autoimmune response. This inflammation can cause the walls of the blood vessels to thicken and narrow, reducing blood flow to various organs and tissues, potentially leading to organ damage. Autoimmune vasculitis can affect any size of blood vessel and can involve multiple organs.
Symptoms
The symptoms of autoimmune vasculitis can vary widely depending on the type and severity of the condition and which organs are affected. Common symptoms include:
- Fever: Persistent low-grade fever.
- Fatigue: Persistent and debilitating tiredness.
- Weight Loss: Unintentional loss of weight.
- Muscle and Joint Pain: Generalized aches and pains.
- Rash: Skin changes, including red or purple spots.
- Nerve Problems: Numbness, tingling, and weakness.
- Breathing Difficulties: Shortness of breath, coughing, and chest pain.
- Gastrointestinal Symptoms: Abdominal pain, nausea, and vomiting.
- Kidney Issues: Blood in the urine and high blood pressure.
When to See a Doctor
Early diagnosis and treatment of autoimmune vasculitis are crucial for managing the condition effectively and preventing serious complications. You should see a doctor if you experience:
- Persistent fever and unexplained weight loss.
- Muscle and joint pain that does not improve with rest.
- Skin rashes or changes.
- Numbness, tingling, or weakness in the limbs.
- Persistent breathing difficulties or chest pain.
- Blood in the urine or gastrointestinal symptoms.
Causes
The exact cause of autoimmune vasculitis is unknown, but it is believed to result from a combination of genetic, environmental, and immune system factors. Potential contributing factors include:
- Genetics: Family history of autoimmune diseases.
- Immune System Malfunction: The immune system mistakenly attacks blood vessel walls.
- Infections: Certain viral and bacterial infections may trigger vasculitis.
- Medications: Some drugs can induce an autoimmune response leading to vasculitis.
Risk Factors
Several factors may increase the risk of developing autoimmune vasculitis, including:
- Age: Some types of vasculitis are more common in certain age groups.
- Sex: Certain types of vasculitis may be more common in either men or women.
- Family History: Higher risk if a close relative has autoimmune diseases.
- Autoimmune Disorders: Having another autoimmune disease increases the risk.
- Infections: Previous infections can increase the risk.
Diagnostics
Diagnosing autoimmune vasculitis involves several steps:
- Medical History and Physical Exam: The doctor will review symptoms and perform a thorough physical examination.
- Blood Tests: To check for markers of inflammation, autoimmune antibodies, and organ function.
- Urine Tests: To detect kidney involvement.
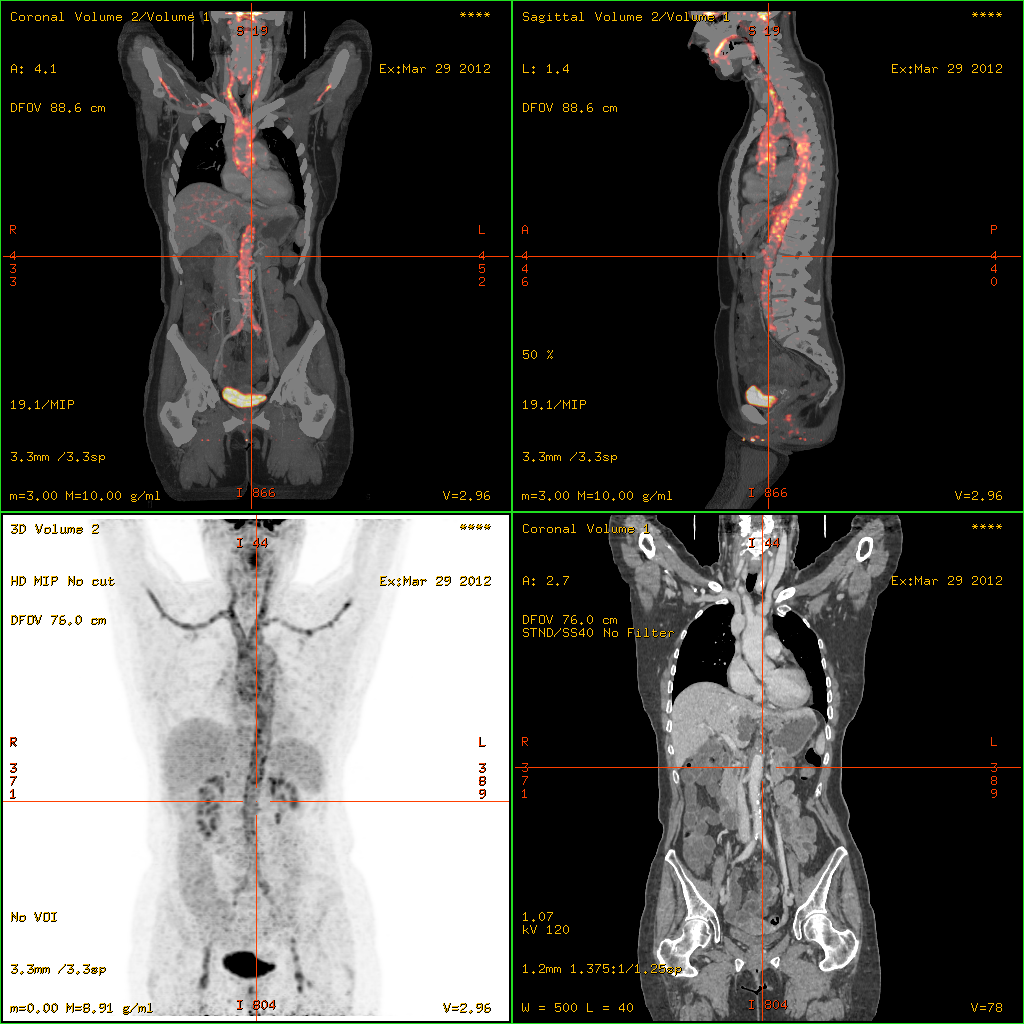
- Imaging Tests: X-rays, CT scans, MRI, or PET scans to assess organ and blood vessel involvement.
- Biopsy: A sample of affected tissue or blood vessel to confirm the diagnosis and assess the extent of inflammation.
Treatment Approaches
There is no cure for autoimmune vasculitis, but various treatment options can help manage symptoms, reduce inflammation, and prevent organ damage. Treatment approaches include:
- Medications:
- Corticosteroids: Such as prednisone to reduce inflammation.
- Immunosuppressants: Such as azathioprine, methotrexate, or cyclophosphamide to suppress the immune system.
- Biologic Agents: Such as rituximab to target specific immune pathways.
- Plasma Exchange (Plasmapheresis):
- Plasmapheresis: To remove antibodies from the blood, particularly in severe cases.
- Surgery:
- Surgical Interventions: To repair or bypass damaged blood vessels in severe cases.
- Lifestyle and Home Remedies:
- Healthy Diet: Eating a balanced diet to support overall health.
- Regular Exercise: Engaging in light to moderate physical activity as tolerated.
- Stress Management: Techniques such as yoga, meditation, and deep breathing to manage stress.
- Smoking Cessation: Quitting smoking to improve vascular health.
- Regular Monitoring: Regular follow-ups with a healthcare provider to monitor symptoms and adjust treatments as needed.
Complications
Autoimmune vasculitis can lead to several complications if not properly managed, including:
- Organ Damage: Damage to organs such as the kidneys, lungs, heart, and brain.
- Blood Clots: Increased risk of blood clots due to inflammation.
- Aneurysms: Weakening of blood vessel walls leading to aneurysms.
- Infections: Increased susceptibility to infections due to immunosuppressive therapy.
- Vision Loss: If blood vessels in the eyes are affected.
Recent Updates
Recent advancements in autoimmune vasculitis research include:
- Biologic Therapies: Development of new biologic drugs targeting specific immune pathways involved in vasculitis.
- Genetic Research: Identifying genetic markers to better understand the genetic basis of vasculitis and develop personalized treatments.
- Improved Diagnostic Techniques: Enhanced imaging and biomarker identification for early detection and monitoring of disease progression.
- Patient Education: Increased efforts to educate patients on the importance of early diagnosis and adherence to treatment plans.
Conclusion
Managing autoimmune vasculitis effectively requires a comprehensive approach that includes medication, lifestyle changes, and regular consultations with healthcare providers. Early diagnosis and intervention are crucial in preventing complications and improving quality of life. Staying informed about the latest research and treatment options can empower individuals to better manage their condition and maintain a good quality of life. If you experience persistent symptoms of autoimmune vasculitis, consult your doctor promptly for a thorough evaluation and appropriate management.
Additional Content
For comprehensive information on the various treatments you can explore our Autoimmune Disease Treatment page. If you are seeking expert medical advice, our Top Autoimmune Doctors section provides a list of highly recommended specialists. Additionally, for an overview of other autoimmune conditions, visit our Autoimmune Diseases page.