Table of Contents
Systemic Lupus Erythematosus (SLE): Symptoms, Causes & Effective Management
This condition, commonly known as Lupus, is a chronic autoimmune disease where the immune system mistakenly attacks healthy tissues, affecting various parts of the body, including joints, skin, kidneys, heart, and brain.

Quick Facts
- Prevalence: Affects approximately 0.1% of the global population.
- Common Symptoms: Joint pain, fatigue, rash.
- Affected Population: Primarily women between the ages of 15 and 45, although it can affect anyone.
Understanding Systemic Lupus Erythematosus
This autoimmune disease occurs when your immune system produces autoantibodies that target your body’s tissues, causing inflammation and potential damage in multiple organ systems. Its symptoms and severity vary greatly among individuals.
Common Symptoms
Early recognition supports effective management and improved outcomes:
- Joint pain and swelling
- Fatigue and fever
- Butterfly-shaped facial rash across the cheeks and nose
- Sensitivity to sunlight (photosensitivity)
- Chest pain and difficulty breathing
- Kidney problems
- Neurological symptoms (headaches, cognitive impairment)
- Hair loss and mouth ulcers
Causes and Risk Factors
The exact cause of Systemic Lupus Erythematosus remains unclear, but multiple factors contribute to its development:
- Genetic Factors: Increased risk with family history of this or other autoimmune disorder.
- Hormonal Influences: Higher incidence in women suggests estrogen involvement.
- Environmental Triggers: Sun exposure, infections, certain medications, or stress.
Diagnosis
Diagnosing lupus involves multiple evaluations:
- Medical History: Detailed analysis of symptoms, medical and family history.
- Physical Examination: Checking joints, skin, and other organs for characteristic signs.
- Laboratory Tests: Blood tests for autoantibodies (ANA, anti-dsDNA), inflammatory markers, and organ function.
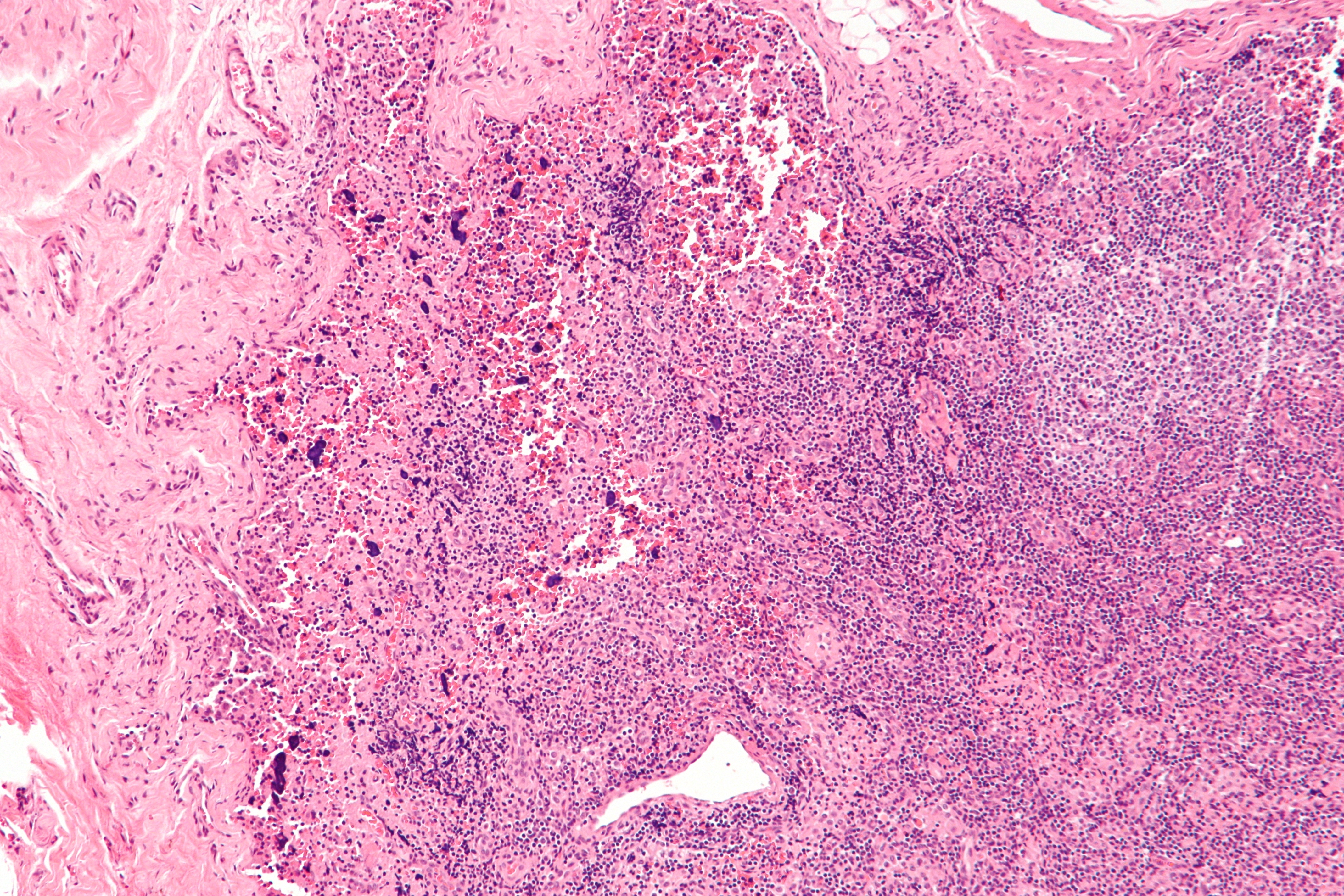
- Imaging and Biopsy: May be performed to assess organ involvement and confirm diagnosis.
Effective Treatments and Management
Lupus management aims to reduce inflammation, control symptoms, and prevent flare-ups:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), antimalarial drugs (hydroxychloroquine), corticosteroids, and immunosuppressants.
- Regular Monitoring: Ongoing medical appointments to monitor organ function and medication effects.
- Lifestyle Adjustments: Sun protection, balanced diet, regular moderate exercise, and stress management.
Potential Complications if Left Untreated
Untreated or poorly managed – this autoimmune disorder can lead to serious, life-threatening complications:
- Kidney failure (lupus nephritis)
- Increased risk of cardiovascular diseases and stroke
- Neurological issues, including seizures or cognitive impairment
- Higher susceptibility to infections
When to See a Doctor
Seek immediate medical attention if experiencing persistent symptoms like joint pain, unexplained rashes, severe fatigue, or any signs of organ involvement (e.g., breathing difficulties, significant swelling). Early intervention greatly improves health outcomes.
Practical Tips for Living with Lupus
Effective daily management involves:
- Adhering strictly to prescribed medications and treatment plans.
- Protecting skin from sun exposure with sunscreen and protective clothing.
- Maintaining regular gentle physical activity (walking, swimming, yoga).
- Employing relaxation techniques such as meditation or mindfulness.
- Building a supportive network through lupus support groups and counseling.
Recent Research and Advances
Advances in research continue to enhance understanding and treatment:
- Development of targeted biological therapies designed to reduce autoimmunity.
- Investigations into genetic and molecular factors to personalize treatments.
- Improved diagnostic methods allowing earlier disease detection and intervention.
Frequently Asked Questions
Is SLE curable? Currently, there is no cure for this disease, but effective treatments can control symptoms and significantly improve quality of life.
Can pregnancy affect lupus symptoms? Yes, pregnancy can affect symptoms, and women with this condition should plan pregnancies carefully with healthcare providers to ensure safety for both mother and baby.
Can lifestyle changes help manage lupus? Yes, adopting a healthy lifestyle—including balanced nutrition, regular exercise, and stress management—can significantly support overall health and symptom control.
Additional Content
For comprehensive information on the various treatments you can explore our Autoimmune Disease Treatment page. If you are seeking expert medical advice, our Top Autoimmune Doctors section provides a list of highly recommended specialists. Additionally, for an overview of other autoimmune conditions, visit our Autoimmune Diseases page.