Table of Contents
Primary Sclerosing Cholangitis (PSC): Symptoms, Causes & Effective Management
Primary Sclerosing Cholangitis (PSC) is a chronic autoimmune liver disease characterized by progressive inflammation and scarring of the bile ducts. This damage can ultimately lead to liver dysfunction, bile duct obstruction, and severe liver complications if not effectively managed.
Quick Facts
- Prevalence: Approximately 1-6 cases per 100,000 people worldwide.
- Common Symptoms: Fatigue, itching, jaundice.
- Affected Population: Primarily affects individuals between the ages of 30 and 50, with a higher prevalence in men.
Understanding Primary Sclerosing Cholangitis
PSC occurs when the immune system mistakenly attacks the bile ducts, causing inflammation and scarring (fibrosis). Over time, the damaged ducts restrict bile flow, which can accumulate and cause progressive liver damage, potentially leading to cirrhosis, liver failure, or liver cancer.
Common Symptoms
Early recognition is crucial for effective management and improved outcomes:
- Chronic fatigue
- Itching (pruritus), which can be severe and persistent
- Jaundice (yellowing of the skin and eyes)
- Abdominal discomfort or pain
- Unexplained weight loss
- Episodes of fever or chills, potentially indicating infection
- Dark urine and pale stools
Symptoms may initially be subtle or intermittent, potentially delaying diagnosis.
Causes and Risk Factors
The precise cause of PSC remains unknown, but several factors are associated with increased risk:
- Autoimmune Disorders: Higher risk with inflammatory bowel disease, particularly ulcerative colitis.
- Genetic Factors: Family history of PSC or other autoimmune disorders may increase susceptibility.
- Environmental Influences: Possible triggers include infections or exposure to toxins.
Diagnosis
Diagnosis of PSC involves a combination of clinical evaluations and diagnostic tests:
- Medical History: Assessment of symptoms, medical history, and family background.
- Physical Examination: Evaluation for jaundice, enlarged liver or spleen, and signs of liver disease.
- Blood Tests: Liver function tests, alkaline phosphatase levels, and autoantibody testing.
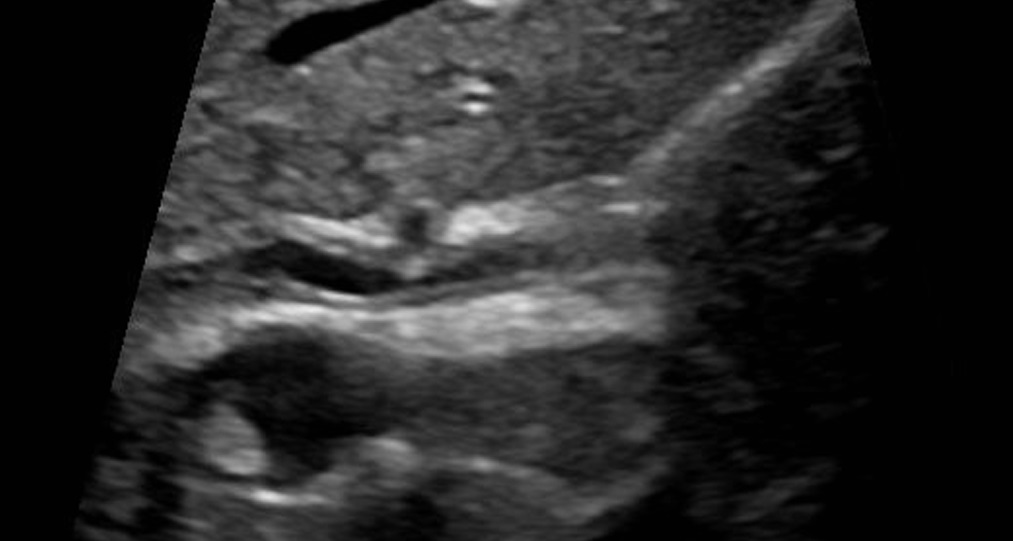
- Imaging Studies: Magnetic resonance cholangiopancreatography (MRCP) to visualize bile duct abnormalities.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): In selected cases, to confirm diagnosis, evaluate strictures, or obtain biopsies.
Effective Treatments and Management
Currently, there is no definitive cure for PSC, but treatment strategies can manage symptoms, prevent complications, and enhance quality of life:
- Medication: Ursodeoxycholic acid (UDCA) for improving bile flow and liver enzyme levels.
- Symptom Management: Medications like cholestyramine for itching relief.
- Endoscopic Therapy: ERCP interventions to dilate narrowed bile ducts or insert stents.
- Regular Monitoring: Frequent medical follow-ups and tests to track disease progression and identify complications early.
- Liver Transplant: Recommended for severe cases with significant liver damage or advanced liver failure.
Potential Complications if Left Untreated
Without adequate management, PSC can lead to serious health issues:
- Liver cirrhosis (irreversible scarring)
- Portal hypertension and associated complications (e.g., variceal bleeding)
- Increased risk of cholangiocarcinoma (bile duct cancer)
- Recurrent bile duct infections (cholangitis)
- Malabsorption and nutritional deficiencies
When to See a Doctor
Seek medical attention if experiencing persistent fatigue, unexplained itching, jaundice, or abdominal discomfort. Early intervention is crucial for slowing disease progression and preventing serious complications.
Practical Tips for Living with Primary Sclerosing Cholangitis
Effective daily management strategies include:
- Strict adherence to medical recommendations and regular health monitoring.
- Maintaining a nutritious diet, rich in vitamins and minerals, and avoiding alcohol.
- Regular exercise to enhance overall health and combat fatigue.
- Effective stress management through meditation, yoga, or counseling.
- Connecting with support groups for emotional encouragement and practical advice.
Recent Research and Advances
Ongoing research continues to improve understanding and treatment of PSC:
- Investigations into genetic and immunological mechanisms underlying PSC.
- Development of novel therapeutic agents aimed at reducing inflammation and fibrosis.
- Improved diagnostic techniques allowing earlier detection and management.
- Studies exploring personalized medicine approaches based on genetic profiles.
Frequently Asked Questions
Is primary sclerosing cholangitis hereditary? Genetic factors may contribute to susceptibility, although direct hereditary transmission is uncommon.
Can PSC be cured? Currently, PSC has no cure, but early diagnosis and effective management can significantly improve quality of life and prognosis.
Does PSC affect life expectancy? Life expectancy can vary greatly, depending on disease severity and treatment effectiveness. Early detection and management greatly enhance outcomes.
Additional Content
For comprehensive information on the various treatments you can explore our Autoimmune Disease Treatment page. If you are seeking expert medical advice, our Top Autoimmune Doctors section provides a list of highly recommended specialists. Additionally, for an overview of other autoimmune conditions, visit our Autoimmune Diseases page.