Table of Contents
Primary Biliary Cholangitis (PBC): Symptoms, Causes & Effective Management
Primary Biliary Cholangitis (PBC), formerly known as primary biliary cirrhosis, is a chronic autoimmune condition affecting the liver. It is characterized by inflammation and gradual destruction of the small bile ducts within the liver, leading to bile accumulation, liver damage, and potentially cirrhosis if untreated.
Quick Facts
- Prevalence: Approximately 40-400 cases per million worldwide.
- Common Symptoms: Fatigue, itchy skin (pruritus), jaundice.
- Affected Population: Primarily affects middle-aged women, usually diagnosed between ages 40-60.
Understanding Primary Biliary Cholangitis
In PBC, the immune system mistakenly targets the bile ducts within the liver, leading to inflammation and scarring (fibrosis). The bile ducts carry bile—a substance crucial for digestion—from the liver to the intestines. Damage to these ducts causes bile to build up, eventually harming liver cells and impairing liver function.
The progressive nature of PBC makes early detection and intervention crucial to prevent severe liver complications.
Common Symptoms
Symptoms of PBC can vary and often develop gradually:
- Persistent fatigue
- Severe itching (pruritus), especially at night
- Jaundice (yellowing of skin and eyes)
- Dry eyes and mouth (often associated with Sjögren’s syndrome)
- Abdominal discomfort or swelling
- Joint and muscle pain
- Dark-colored urine and pale stools
- Elevated cholesterol levels
- Bone and joint pain, indicating potential osteoporosis
Some individuals may have minimal or no symptoms initially, with diagnosis occurring during routine blood tests.
Causes and Risk Factors
The exact cause of PBC remains unknown, though several factors increase the risk:
- Genetic Predisposition: Family history of PBC or other autoimmune diseases.
- Autoimmune Associations: Higher incidence among individuals with thyroid disorders, rheumatoid arthritis, or Sjögren’s syndrome.
- Environmental Triggers: Possible factors include infections, chemical exposures, or lifestyle elements, although no specific trigger has been definitively identified.
Diagnosis
Diagnosing PBC involves a combination of clinical evaluation and specific tests:
- Medical History: Detailed review of symptoms, family history, and previous autoimmune conditions.
- Physical Examination: Assessing signs of liver disease such as jaundice, enlarged liver or spleen, and skin conditions.
- Blood Tests: Liver function tests (alkaline phosphatase, bilirubin), and detection of antimitochondrial antibodies (AMA), specific to PBC.
- Imaging Tests: Ultrasound or MRI scans to evaluate liver structure and detect bile duct abnormalities.
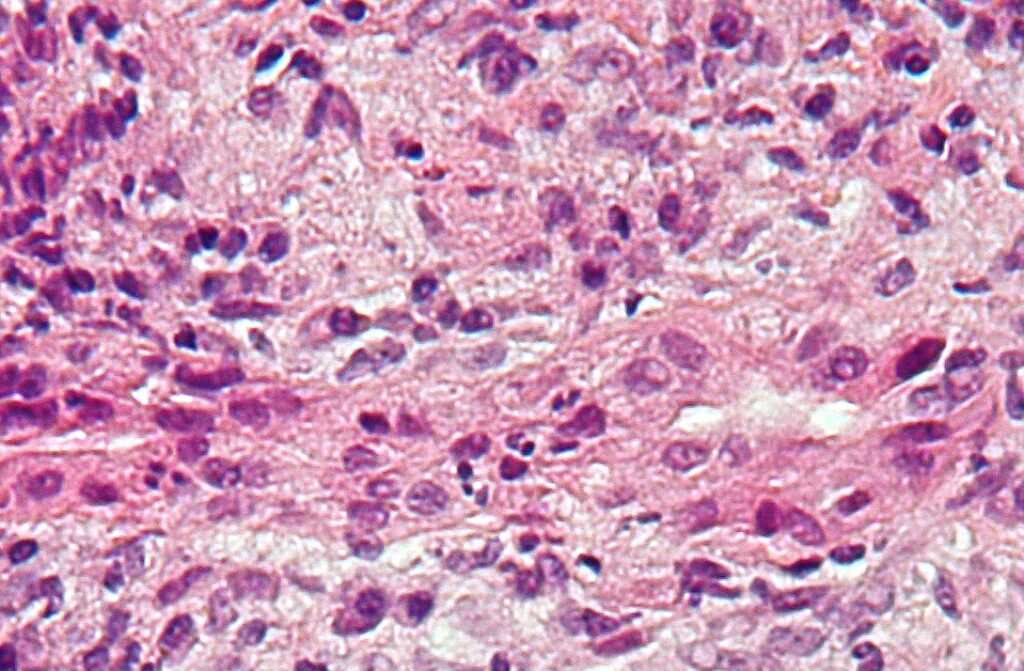
- Liver Biopsy: Often used to confirm diagnosis, assess disease severity, and plan appropriate treatment.
Effective Treatments and Management
Currently, no cure exists for PBC, but treatments effectively slow disease progression, relieve symptoms, and prevent complications:
- Medication: Ursodeoxycholic acid (UDCA) is the primary treatment, improving liver function and reducing inflammation. Obeticholic acid may be prescribed if UDCA is insufficient.
- Symptom Management: Antihistamines, cholestyramine, or rifampicin for severe itching; artificial tears and saliva substitutes for dry eyes and mouth.
- Bone Health: Supplements and medications (vitamin D and calcium) to prevent osteoporosis.
- Regular Monitoring: Frequent check-ups and blood tests to assess liver function and response to treatment.
- Liver Transplant: Recommended in advanced cases of liver failure or severe liver damage.
Potential Complications if Left Untreated
Untreated PBC can lead to severe complications, significantly impacting health and life expectancy:
- Liver cirrhosis (severe scarring)
- Portal hypertension, causing fluid accumulation (ascites) and varices
- Osteoporosis and increased risk of fractures
- Vitamin deficiencies due to impaired bile flow
- Increased risk of liver cancer (hepatocellular carcinoma)
When to See a Doctor
It’s important to consult your healthcare provider promptly if experiencing unexplained fatigue, persistent itching, jaundice, or other concerning symptoms. Early diagnosis and management of PBC significantly improve outcomes and quality of life.
Practical Tips for Living with Primary Biliary Cholangitis
Living well with PBC includes making proactive lifestyle choices:
- Consistently adhere to medication schedules and healthcare recommendations.
- Maintain a balanced, nutritious diet low in sodium, and avoid alcohol to protect liver function.
- Engage in moderate, regular exercise to enhance overall health and combat fatigue.
- Prioritize bone health with appropriate supplements and regular physical activity.
- Join support groups or online communities for emotional support and practical advice.
Recent Research and Advances
Significant advances continue to improve the management and understanding of PBC:
- Development of new therapeutic drugs to control symptoms and slow liver damage.
- Research into genetic markers for better disease prediction and tailored treatment.
- Improved non-invasive diagnostic and monitoring techniques.
- Studies exploring immune system modulation and personalized medical interventions.
Frequently Asked Questions
Is Primary Biliary Cholangitis hereditary?
While not strictly hereditary, genetic factors can increase the likelihood of developing PBC, especially in families with autoimmune disorders.
Can Primary Biliary Cholangitis be cured?
Currently, there is no cure, but available treatments effectively manage symptoms and slow disease progression.
What lifestyle changes can help manage PBC?
Dietary adjustments, regular exercise, limiting alcohol, and careful medication adherence are essential for managing PBC effectively and improving overall health outcomes.
Additional Content
For comprehensive information on the various treatments you can explore our Autoimmune Disease Treatment page. If you are seeking expert medical advice, our Top Autoimmune Doctors section provides a list of highly recommended specialists. Additionally, for an overview of other autoimmune conditions, visit our Autoimmune Diseases page