Table of Contents
Understanding Polymyalgia Rheumatica (PMR)
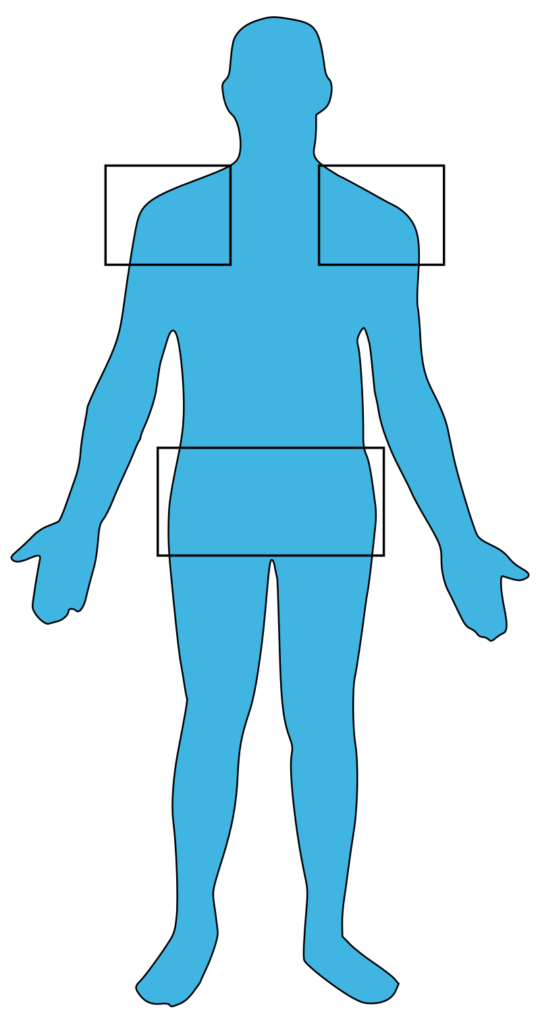
Polymyalgia rheumatica (PMR) is an inflammatory disorder that primarily affects older adults, causing muscle pain and stiffness, especially in the shoulders and hips. The exact cause of PMR is unknown, but it is believed to be related to immune system dysfunction. Polymyalgia Rheumatica can significantly impact daily activities due to pain and stiffness, particularly in the morning or after periods of inactivity.
Symptoms
The symptoms of PMR can develop suddenly or gradually and typically include:
- Muscle Pain: Aching and pain in the shoulders, neck, upper arms, hips, and thighs.
- Stiffness: Severe stiffness, particularly in the morning or after resting.
- Limited Range of Motion: Difficulty moving the affected areas due to pain and stiffness.
- Fatigue: Persistent tiredness and lack of energy.
- Fever: Low-grade fever.
- Weight Loss: Unintentional weight loss.
- Depression: Feelings of sadness or depression due to chronic pain and discomfort.
When to See a Doctor
Early diagnosis and treatment of Polymyalgia Rheumatica are crucial for managing the condition effectively and preventing complications. You should see a doctor if you experience:
- Persistent muscle pain and stiffness, especially in the shoulders and hips.
- Difficulty moving or performing daily activities due to pain.
- Unexplained weight loss and fatigue.
- Symptoms that significantly impact your quality of life.
Causes
The exact cause of Polymyalgia Rheumatica is unknown, but it is believed to involve a combination of genetic and environmental factors. Potential contributing factors include:
- Genetics: Family history of Polymyalgia Rheumatica or other autoimmune conditions.
- Immune System Dysfunction: The immune system may attack the body’s tissues, leading to inflammation.
- Environmental Triggers: Infections or other environmental factors may trigger the onset of PMR.
Risk Factors
Several factors may increase the risk of developing PMR, including:
- Age: Most commonly affects individuals over the age of 50.
- Sex: Women are more likely to develop PMR than men.
- Ethnicity: More common in people of Northern European descent.
- Genetics: Family history of this or other autoimmune conditions.
Diagnostics
Diagnosing PMR involves several steps:
- Medical History and Physical Exam: The doctor will review symptoms and perform a thorough physical examination.
- Blood Tests: To check for markers of inflammation, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
- Imaging Tests: Ultrasound or MRI may be used to detect inflammation in the shoulders, hips, and other affected areas.
- Response to Treatment: A rapid improvement of symptoms with low-dose corticosteroids can help confirm the diagnosis.
Treatment Approaches
There is no cure for PMR, but various treatment options can help manage symptoms and reduce inflammation. Treatment approaches include:
- Medications:
- Corticosteroids: Such as prednisone to reduce inflammation and relieve symptoms.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): To help manage pain and inflammation.
- Calcium and Vitamin D Supplements: To prevent bone loss due to long-term corticosteroid use.
- Lifestyle and Home Remedies:
- Exercise: Gentle exercises and physical therapy to maintain joint flexibility and muscle strength.
- Healthy Diet: Eating a balanced diet rich in calcium and vitamin D to support bone health.
- Stress Management: Techniques such as yoga, meditation, and deep breathing to manage stress.
- Regular Monitoring: Regular follow-ups with a healthcare provider to monitor symptoms and adjust treatments as needed.
Complications
PMR can lead to several complications if not properly managed, including:
- Giant Cell Arteritis (GCA): An inflammatory condition affecting the arteries in the head, which can cause severe headaches, vision problems, and jaw pain.
- Bone Loss: Osteoporosis due to long-term corticosteroid use.
- Decreased Quality of Life: Chronic pain and stiffness can significantly impact daily activities and overall well-being.
Recent Updates
Recent advancements in PMR research include:
- Improved Diagnostic Tools: Development of more precise tests to detect early markers of inflammation and diagnose PMR.
- Genetic Research: Identifying genetic markers to better understand the genetic basis of PMR and develop personalized treatments.
- New Medications: Exploring new anti-inflammatory drugs and biologics to treat PMR more effectively with fewer side effects.
- Patient Education: Increased efforts to educate patients on the importance of early diagnosis, treatment adherence, and lifestyle modifications to manage PMR effectively.
Conclusion
Managing Polymyalgia Rheumatica effectively requires a comprehensive approach that includes medication, lifestyle changes, and regular consultations with healthcare providers. Early diagnosis and intervention are crucial in preventing complications and improving quality of life. Staying informed about the latest research and treatment options can empower individuals to better manage their condition and maintain a good quality of life. If you experience persistent symptoms of PMR, consult your doctor promptly for a thorough evaluation and appropriate management.
Additional Content
For comprehensive information on the various treatments you can explore our Autoimmune Disease Treatment page. If you are seeking expert medical advice, our Top Autoimmune Doctors section provides a list of highly recommended specialists. Additionally, for an overview of other autoimmune conditions, visit our Autoimmune Diseases page.